Modern-day fertility treatments have made families a reality for individuals and couples struggling with infertility, with thousands of global organizations helping parents conceive. Thanks to much scientific advancement in the 21st century, we now have modern-day In Vitro Fertilization (IVF) to support individuals on their path toward parenthood.
According to a report published in April 2023 by the World Health Organization (WHO), around 17.5% of the adult population, or 1 in 6 worldwide, experience infertility in their lifetime. This translates to hundreds of millions of individuals globally facing challenges related to conception and family building, indicating that infertility is a significant global health challenge.
In the United States, data from the National Survey of Family Growth (NSFG) suggests that around 9% of women and 9% of men of childbearing age experience infertility. This translates to up to 12.5% of heterosexual couples being affected. However, these figures do not account for LGBTQ+ couples or single individuals who may also face infertility challenges.
What Is In Vitro Fertilization (IVF)?
In Vitro Fertilization, or IVF, is an assisted reproductive technology (ART) that helps individuals or couples conceive.
The process involves stimulating the ovaries with hormonal medications to produce multiple eggs, retrieving the eggs through an egg retrieval procedure, and collecting a sperm sample from the male partner or a donor. The eggs are fertilized with the sperm in a lab, and the resulting embryos are cultured for a few days.
One or more high-quality embryos are then transferred into the uterus, followed by a pregnancy test two weeks later. IVF is used for various reasons, including blocked or damaged fallopian tubes, male infertility, unexplained infertility, age-related infertility, genetic disorders, and fertility preservation for cancer patients.
Learn more from fertility specialist, Dr. Sahakian:
There are many ways to tailor the In Vitro Fertilization process to intended parents, from reciprocal IVF for lesbian couples, to mini IVF treatments for people searching for a lower-impact, less expensive approach to fertility.
IVF has helped many couples with fertility issues successfully conceive, and may be right for you if you have or experience:
- Damaged, blocked, or removed fallopian tubes
- Ovulation disorders, uterine fibroids, or premature ovarian failure
- Decreased sperm count or decreased sperm motility
- Unexplained infertility
Additionally, those who are in a same-sex relationships or are intended single parents can achieve their dream of building a family through IVF.

When To Use IVF As Fertility Treatment
Since its introduction in the 1980s, in vitro fertilization (IVF) has revolutionized reproductive medicine, leading to the birth of nearly 10 million babies through assisted reproductive technology (ART). However, it's important to understand that IVF doesn't guarantee a successful pregnancy. While some patients may conceive with their first cycle, others may require multiple attempts, and for some, pregnancy may remain elusive.
Good Candidates for IVF
- Women with blocked or damaged fallopian tubes
- Women with ovulation disorders (e.g., PCOS (Polycystic Ovary Syndrome)
- Women with endometriosis or uterine fibroids
- Women with premature ovarian failure (POI) or age-related infertility
- Men with low sperm count, motility issues, or abnormal sperm morphology
- Couples with unexplained infertility after thorough testing
- Couples with genetic disorders who wish to screen embryos
- Same-sex couples or single individuals using donor sperm/eggs
When IVF May Not be Effective
Individuals with serious underlying health conditions that could be exacerbated by pregnancy or those who haven't explored other less invasive fertility treatments may not be ideal candidates for IVF. Additionally, those who are not emotionally or financially prepared for the potential challenges and costs associated with IVF should consider other options. The following are candidates should discuss their situation with a fertility specialist:- Women over 40 years of age (it’s urgent you act quickly for IVF or fertility preservation)
- Women with severe medical conditions that could make pregnancy risky
- Individuals with untreated mental health issues that could impact parenting
- Those with unrealistic expectations about IVF success rates
- Individuals who are not financially or emotionally prepared for the process
Because IVF is unique to each patient’s situation, there is no “one-size-fits-all” approach to treatment. However, medications, blood tests, vaginal ultrasounds, sperm and egg retrieval, fertilization and embryo transfer are all critical elements of the process.
IVF Process
The IVF treatment process is a complex journey, both emotionally and physically. It's natural to experience a mix of hope, anxiety, and stress. Understanding what to expect can help you prepare emotionally and seek support when needed. The physical demands of IVF, like hormone injections and procedures, can also be challenging. Knowing what's involved helps you manage side effects and feel more in control. It's also wise to be upfront about the financial commitment so you can plan accordingly.
Being informed empowers you to make the right choices for you and your partner. This includes decisions about embryo transfer, genetic testing, and setting realistic expectations about success rates. Knowledge is key, so ask questions, advocate for your needs, and take an active role in your IVF journey.
The IVF process has many elements:

1. Consultation and Testing
When the IVF cycle begins, your clinic will order a number of pre-treatment tests. Some tests are mandated by state and federal law, while testing required by your clinician is customized to you. These tests often include a baseline ultrasound, bloodwork, and a semen analysis for the male partner to assess your fertility challenges and possibilities. However, other tests may also be required.
2. Ovarian Stimulation
Ovarian stimulation is a critical part of egg production. By using fertility medications, women can prepare for egg retrieval and increase their chances of a successful pregnancy. Oral and injectable fertility medications are often recommended in addition to hormones for optimal results. This may be conducted with a transvaginal ultrasound to determine when the eggs have matured.
3. Egg Retrieval
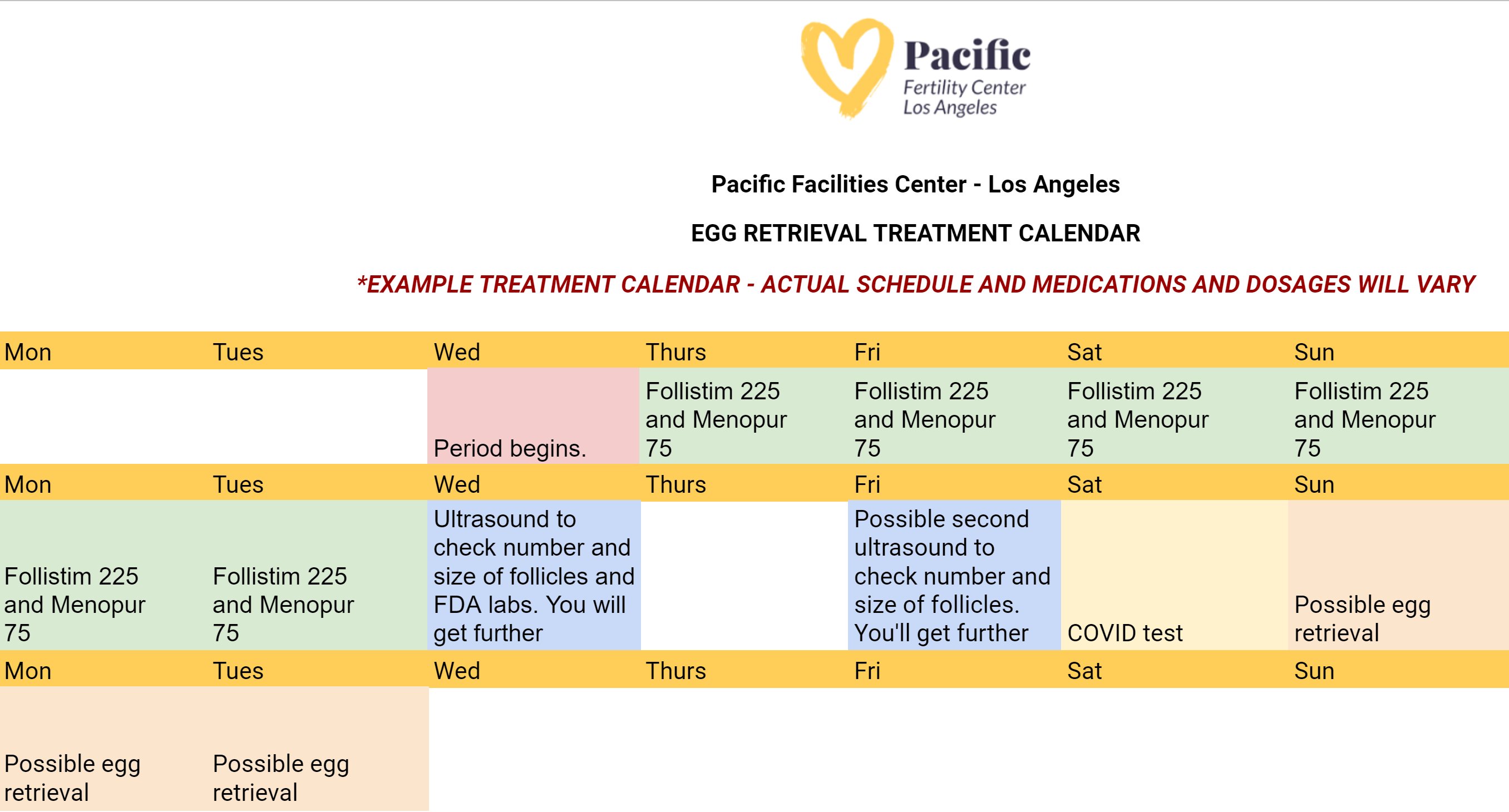
During the egg retrieval process, patients will receive general anesthesia to sleep during the procedure. Next, the eggs are then retrieved by placing a needle through the vaginal wall and into the ovary––and suctioned from the growing follicles and collected into test tubes. Finally, the test tubes are passed to the waiting embryologist. Here's what the egg retrieval calendar might look like:
4. Fertilization
Once the eggs are in the laboratory, they will be visualized under a microscope and prepared for fertilization with either fresh or frozen sperm. A process called ICSI or Intracytoplasmic Sperm Injection is then performed to inject one healthy sperm into each of the viable eggs.
5. Embryo Freezing and Genetic Testing
The following morning, the embryologist will be able to determine how many embryos have formed. The embryos will typically spend 5-7 days in the laboratory before they are ready to be frozen, or transferred back to the uterus. Frozen embryos tend to have better success rates. Most patients will choose to test embryos for genetic or chromosome abnormalities prior to embryo transfer through preimplantation genetic screening.
6. Embryo Transfer
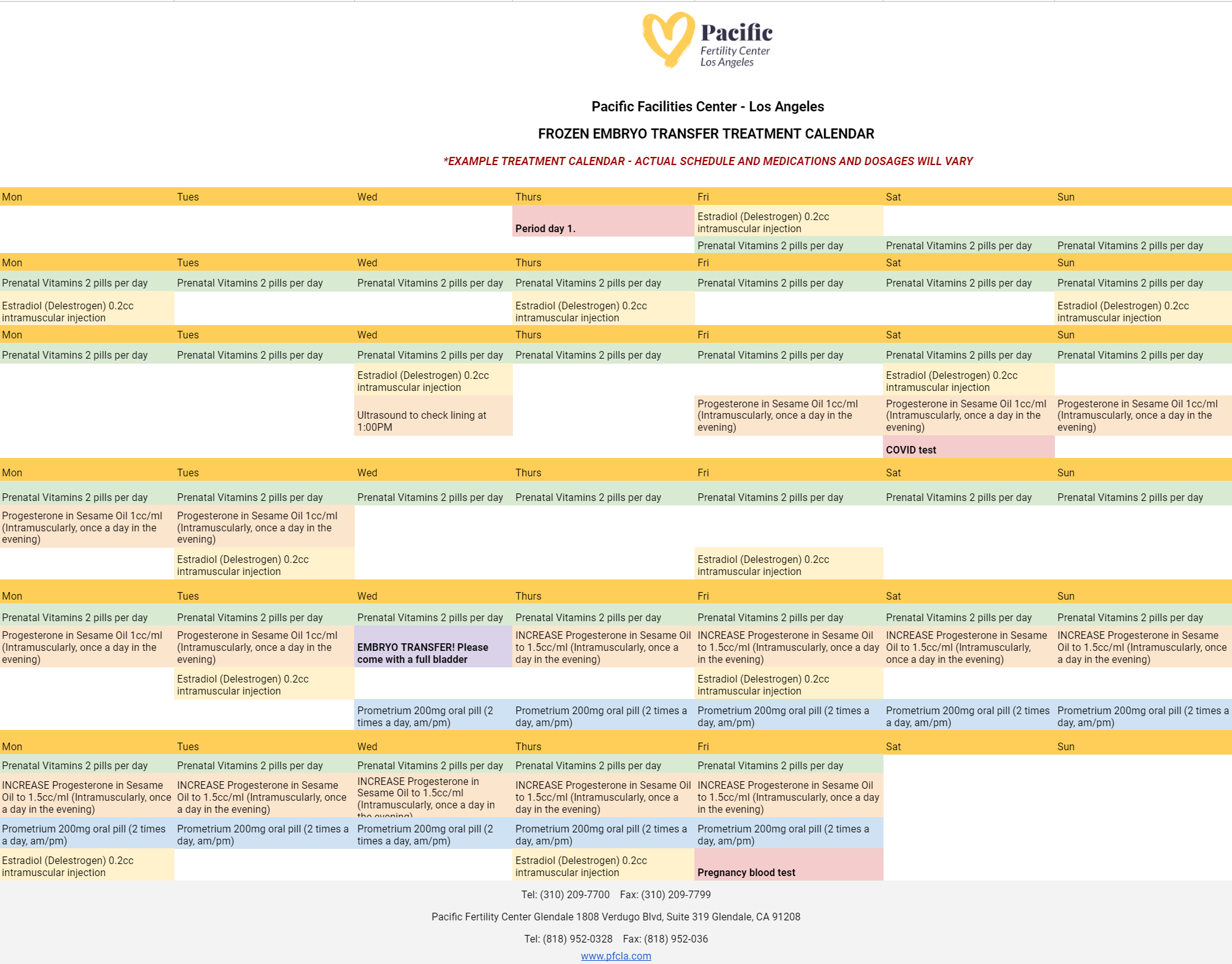
Preparing for your embryo transfer is one of the most important processes in your IVF journey. Patients at PFCLA may receive an IVF embryo transfer calendar that resembles the following:
On the day of embryo transfer, the embryos will be graded based on their cell growth and development. This grading system, along with the patient’s age, will help the physician and patient to decide on the appropriate number of embryos to transfer.
An embryo transfer procedure feels similar to a pap smear and is performed while the patient is awake. To start, the cervix is visualized and cleaned. Then, a very thin catheter (tube) loaded with the embryo(s) is placed gently through the cervix and into the uterine cavity. The embryo(s) are placed near the top of the uterus using ultrasound guidance.
7. Pregnancy Test (Two Weeks After the Embryo Transfer)
Two weeks after an embryo transfer, a blood test is conducted to determine pregnancy. A small sample is drawn from the patient and sent to a lab for analysis of human chorionic gonadotropin (hCG) levels. If hCG is detected above a certain level, it confirms pregnancy. If not, it means the embryo did not implant. In case of a positive result, further tests and ultrasounds are scheduled to monitor the pregnancy. If negative, the patient discusses the next steps with their fertility specialist.
IVF vs. IUI
There are multiple available fertility treatments available today, but some are less effective than others depending on the patient's situation. It’s important to talk to your doctor about what will deliver the best chances of pregnancy, so you’re not wasting precious time and money on options that may not be right for you. IUI, or intrauterine insemination, is one of these treatment options that some use because it is minimally invasive, but the success rates are usually far lower than that of IVF.
After experiencing failed IUIs, many patients turn to IVF as a more reliable fertility treatment. IVF, or in vitro fertilization, oversees most of the stages of conception to increase the chance of a successful pregnancy. Although IUI is a viable and successful fertility treatment option, it is not uncommon for a patient’s first IUI attempt to fail.
But for most who are experiencing infertility, IUI is an inferior option to IVF because IUI acts only as an assistant to natural conception. For many patients seeking fertility treatment, it can be impossible to achieve pregnancy through IUI, and your doctor may recommend starting with IVF.
How To Prepare for Your IVF Treatment
To prepare for IVF, intended parents will likely need various screenings--semen analysis, uterine exams, ovarian reserve testing, and even a mock embryo transfer. This is critical to your individual IVF success, and everyone’s process will look slightly different. Preparing for IVF requires consideration of your diet, blood testing, exercise, stress, and overall health.
Before undergoing IVF, your blood work will be used to assess the level of follicle-stimulating hormone (FSH) in your system. This will give the fertility specialist an understanding of the quality and number of eggs you may have. Also, the blood work performed can help note possible incompatibilities between a mother’s blood type and father’s blood type. This blood work is also crucial in determining the presence of potential genetic disorders, viruses, and diseases that could affect the mother or baby’s health if pregnancy is achieved.
Without critical data from ultrasounds and blood work during the IVF process , the chances of a successful pregnancy are much lower, and fertility specialists can’t use the most modern techniques to truly aid patients in their journey to having a child. Additional testing may be part of the IVF process, depending on the challenges you’ve faced in getting pregnant.
After the embryo transfer, a blood test will be used to measure the pregnancy hormone levels of human chorionic gonadotropin in a woman’s system. The presence of this hormone confirms pregnancy and is typically tested for 11-12 days after an embryo transfer has been performed.
Fertility Medications and IVF
During IVF, it’s common for fertility doctors to prescribe various fertility medications to their female patients as part of the treatment process.
These fertility drugs are meant to trigger the release of various hormones and to regulate ovulation. By doing this, women are in essence made more fertile during the procedure, which improves the chances of pregnancy.
There are common fertility drugs that may be prescribed:
- Follicle-Stimulating Hormone (FSH) - Additional FSH may be used in addition to clomiphene to help stimulate the production of eggs.
- Human Menopausal Gonadotropin (hMG) - A combination of FSH and LH, and can also be used to supplement the effects of clomiphene.
- Human Chorionic Gonadotropin (hCG) - Used to trigger a woman’s ovaries to release viable eggs.
- Clomid or Serophene (Clomiphene) - A type of estrogen-blocking medication. It triggers the release of GnRH (gonadotropin-releasing hormone), FSH (follicle-stimulating hormone), and LH (luteinizing hormone), which signal your ovaries to produce eggs.
The exact medications and types of drugs required for your treatment will be determined during the consultation process. Keep in mind that some of these medications can be taken orally while others will be administered through injections.
Whatever drugs a patient requires, the effectiveness of these medications will require precise timing. Patients should take their fertility drugs as directed by their fertility specialist.
All fertility visits must also be attended on schedule to ensure optimal results. The improper dosage or administration of a fertility drug can result in a failed IVF cycle or reduced potential for a successful pregnancy.
IVF Treatment Side Effects
Fertility drugs used during IVF can increase progesterone levels, leading to fatigue. Stress and anxiety, often present due to past infertility struggles, can exacerbate this fatigue. Open communication with your fertility specialist is crucial to address concerns and access emotional support resources like therapy, support groups, or connecting with couples who have successfully undergone IVF.
While IVF medications can cause various side effects, the potential of starting a family often outweighs these temporary discomforts. Remember, these IVF side effects are common and can be managed to minimize discomfort.
- Mild cramping and bloating
- Fatigue
- Breast tenderness
- Constipation
- Leaking a small amount of clear or blood-tinged fluid after the procedure
- Headaches
- Mood swings
- Hot flashes
However, more severe risks and complications associated with IVF can include:
These complications can bring side effects that should not be ignored. If you're experiencing the following, reach out to your doctor immediately:
- Pelvic pain
- Blood in urine
- Heavy vaginal bleeding
- A fever over 100.5° F
IVF Success Rates and Outcomes
When evaluating IVF success rates, consider age as a significant factor. Look for clinics that transparently report verified success rates and compare them to national averages. Ask your fertility specialist for a personalized estimate. Focus on live birth rates and consider the number of embryos transferred. Cumulative success rates can offer a broader perspective. Choose a transparent clinic and discuss these factors with your specialist for informed decision-making. The Society for Assisted Reproductive Technology (SART), the leading organization for IVF professionals, is an excellent resource for intended parents, offering a helpful success prediction tool on their website.
By having a conversation with your doctor about what you can expect, you’ll know what will and won’t be possible throughout your fertility journey. When it comes down to how many embryos will be implanted and what’s safe for you or your surrogate, trust your doctor’s counsel and let him guide you on the right path.
- The success rate of IVF has improved dramatically since 1985. In the early days of IVF, success rates hovered around 10-15%. Today, the success rate for women under 35 can reach upwards of 55%. This represents a significant increase of approximately 266.7% since the technology was first introduced.
- The Centers for Disease Control and Prevention (CDC) recorded 413,776 fertility treatment cycles in America in 2021. Of that number, 99 percent of fertility treatments involved in vitro fertilization (IVF).
- The overall median age for women undergoing ART is 36.4, an increase of 1.4 years since 2015.
- The CDC reports 186,157 ART cycles in which an embryo was transferred. Of these, 97,128 resulted in live births, up 33% since 2015.
Out of 118,000 cycle starts from intended egg retrievals including all embryo transfers recorded by SART performed in the United States in 2020, under 29% resulted in live births. By contrast, PFCLA has a 44%+ live birth rate from cycle start per intended egg retrieval including all embryo transfers.
Bear in mind that comparing clinics to one another is rarely an ‘apples to apples’ comparison, as different clinics and the physicians therein take different profiles of patients based on age, risk factors and services offered (whether an egg donor was used etc.…). The best thing you can do to understand your personal IVF profile is consult with a physician.
Begin Your IVF Journey With Top-Rated Fertility Care
Building a family has never been more accessible and successful than ever. If you’re coping with infertility blues or looking to start your family but don’t know how, you don’t have to wait any longer to take steps toward this dream.
The fertility specialists at Pacific Fertility Center would be happy to answer any further questions you may have regarding in vitro fertilization (IVF) and your surrogacy options. Contact us to get started today.
Note: This is not intended to be a substitute for professional medical advice, diagnosis or treatment. Information provided is for general educational purposes only and is subject to change without notice. Speak to your doctor directly with any questions you may have regarding a medical condition. Any information contained herein does not replace any care plan as determined by a physician.
You May Also Like
These Stories on In-Vitro Fertilization


.png)
