.jpg?width=5760&name=man-comforting-pregnant-woman-ward-min%20(1).jpg)
Experience an IVF cycle program like no other with a team of doctors that has performed more than 10,000 IVF procedures for intended parents from over 75 countries.
Our doctors know the ups and downs that can occur with the IVF process and will be with you every step of the way to help give you the gift of a beautiful family.
Discover the best personalized attentive care. You’ll see the same team of nurses and doctor, from a dedicated clinical coordinator that organizes and oversees your entire IVF cycle.
Feel confident knowing you’ll leave with your newest family member with our Unlimited Plan. You’ll feel supported by everyone from knowledgeable, empathetic doctors to staff available at any hour to answer any question. Terms and conditions apply. Approval required.
Learn about the different steps you or your partner may take while going through an IVF cycle program here at Pacific Fertility Center Los Angeles.
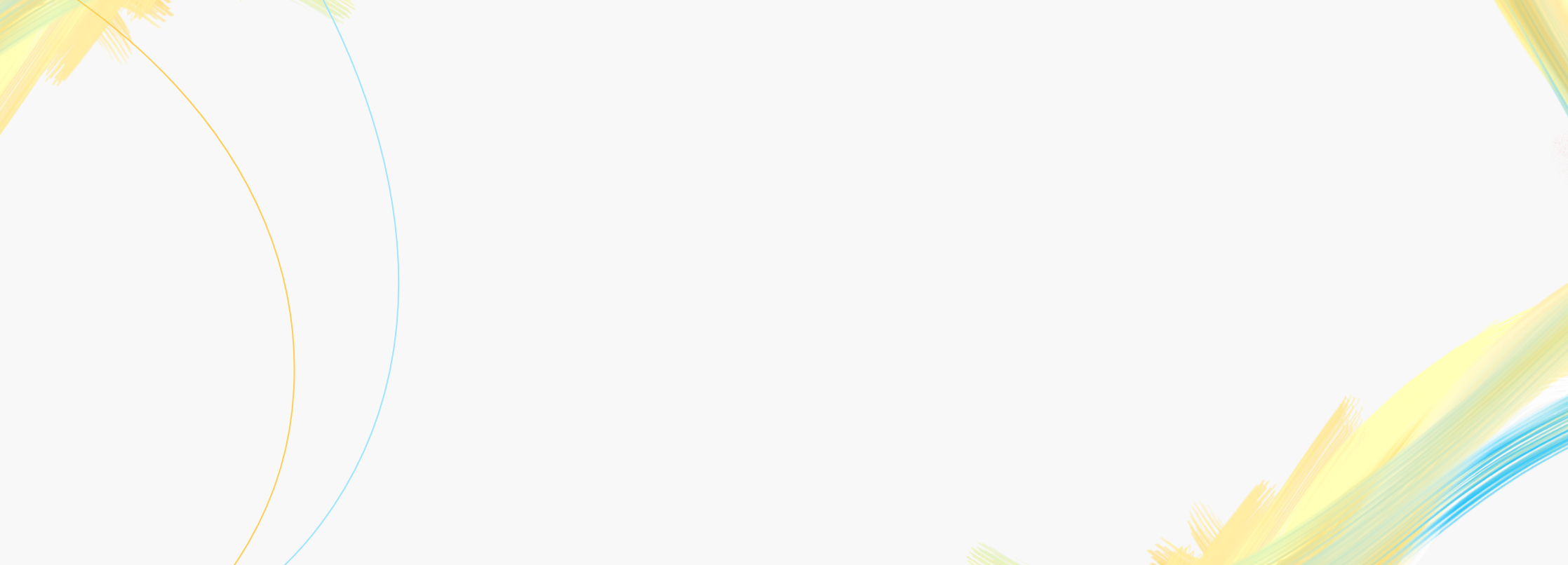
After you choose your PFCLA doctor and go through financial clearance, you or your partner will be assigned to your own personal dedicated care coordinator from the start of your IVF cycle to the very end. Here’s an example of what you can expect during an IVF cycle at PFCLA --Every program is carefully crafted to fit your needs, so your treatment plan may vary.
Your initial IVF cycle appointment will review the overall process and details such as any necessary testing requirements and the medications you’ll need.
Learn more about the initial consultation ➜
Your financial coordinator will guide you through your different pricing package options around the time of your initial consultation. You can connect with your financial coordinator before speaking with a doctor, or you may first want the doctor’s advice on which IVF package is the best fit for you. We have a variety of options for you to choose from, so you can decide if you want to focus on reducing your cost or paying a little extra for more peace of mind.
Learn more about our pricing ➜
After financial clearance, you will be introduced to your clinical care coordinator. Your coordinator will then reach out to you and, if applicable, your egg donor with the next steps to get your journey started.
Your care coordination team will get you set up with everything you need for your (or your egg donor’s) upcoming egg retrieval. They will handle all of your appointments, help with any travel questions, walk you through medication administration, and anything else necessary to set you or your egg donor up for a great retrieval.
Appointments leading up to the egg retrieval could include, but are not limited to, ultrasounds and bloodwork to help determine the number and size of follicles present in your ovaries. Your treatment will be crafted by your doctor especially for you, so every plan looks different. Here's an example of your egg retrieval calendar:
Learn more about the appointments ➜
The egg retrieval procedure is a 10-30 minute process of removing eggs from the ovaries, typically under general anesthesia. Your chances of pregnancy usually increase if your, or your egg donor’s, ovaries produce more eggs. The number of eggs produced depends on many factors, including your or your egg donor’s age and ovarian reserve.
|
In general, women below 35 produce between 10 to 20 more eggs than women over 35—who typically produce less than 10 eggs. |
|
Learn more about the egg retrieval procedure ➜
A fresh or frozen semen sample is provided to our IVF lab (either through a donor or from your partner). For fresh samples, it’s provided the same day as the retrieval. Using that sample, our embryology team fertilizes the eggs and creates embryos.
For IVF, intracytoplasmic sperm injection (ICSI) is often used to create the embryos. ICSI is a process whereby your embryologist injects a single selected sperm into each of the eggs. After the eggs are fertilized, your embryologist checks the eggs to determine if the fertilization was successful, as not every egg gets fertilized.
Depending on what you decide, any embryos leftover can undergo additional treatment. This includes the optional biopsies for genetic screening, until it’s ready to be frozen or transferred.
|
We typically expect a 60 - 80% fertilization rate. |
|
Learn more about the egg fertilization process ➜
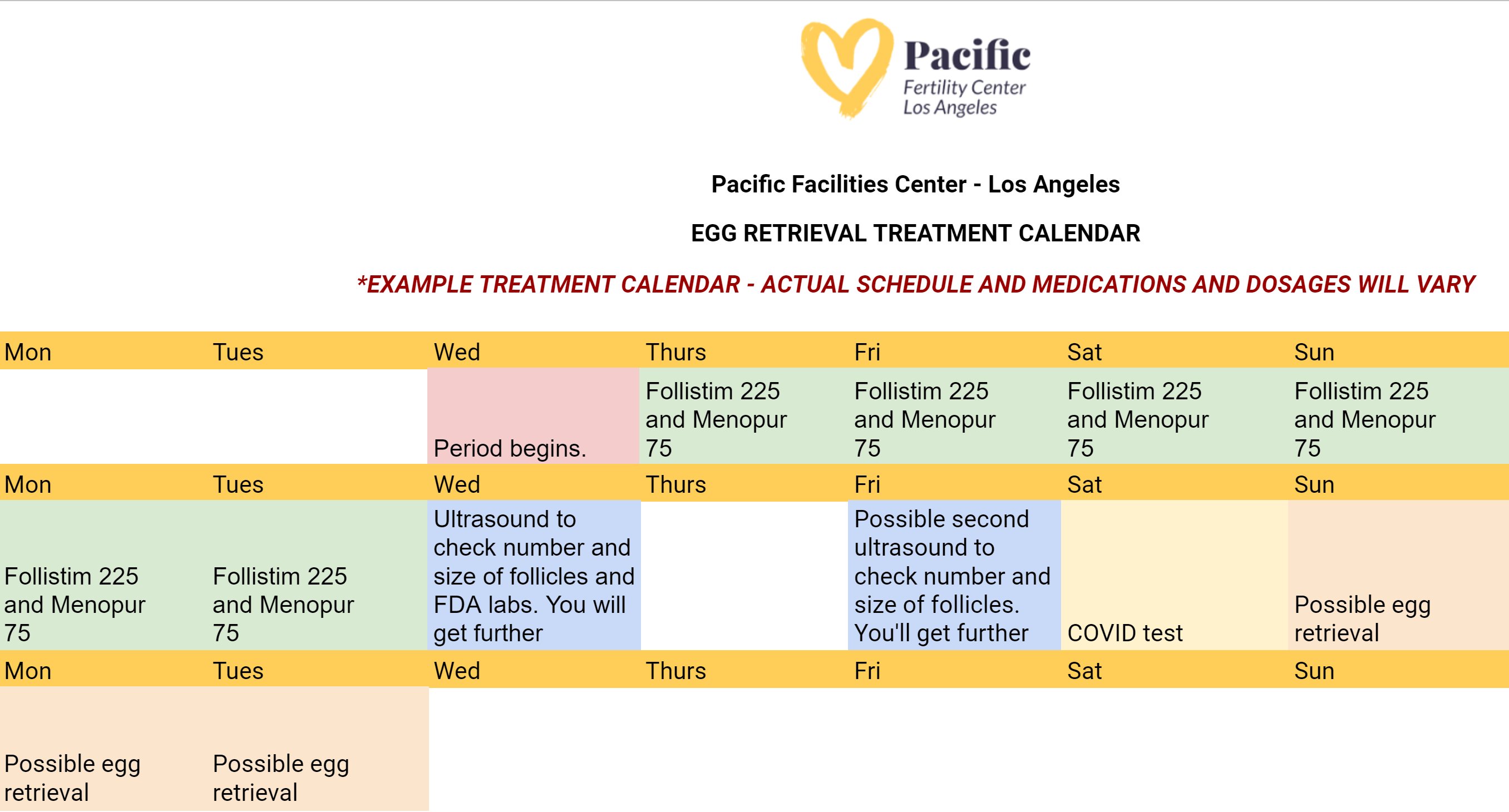
The embryo transfer procedure is one of the final stages of the IVF process. This is the procedure where your doctor places one or more embryo(s) in your or your surrogate’s uterus to create a pregnancy. The exact timing of the transfer depends on where the body is in its cycle, and the preparation of the uterine lining through medications. The success of the transfer depends on many factors, including but not limited to:
Here's what your embryo transfer calendar might look like at PFCLA. Note that medications and timing will be different for each patient.
What is IVF?
Intended parents are in good hands at PFCLA. Realize your dreams of building a family with a variety of fertility services, and feel confident you’ll be supported throughout this journey.
.jpg)
Discover the different forms of male infertility treatments you or your partner can use along with a promising solution for egg fertilization: Intracytoplasmic Sperm Injection (ICSI).
.jpg)
Understand your obstacles and solutions when planning for pregnancy with careful analysis and testing performed by your doctor. From ultrasounds to hormonal testing, you’ll be carefully guided as you evaluate your options.
-min.jpg)
Preserve you or your partner's fertility by freezing healthy eggs for the best chance of a successful pregnancy when you’re ready.
If you’re hoping to start a family, you’ve come to the right place. Our success rates are among the best in the nation. With over 7,000+ babies babies born, our success rate is 40% higher than the national average.
Start your journey toward parenthood by contacting us today.
Fertility Services
Why PFCLA
Resources
Subscribe to our newsletter
Note: This is not intended to be a substitute for professional medical advice, diagnosis or treatment. Information provided is for general educational purposes only and is subject to change without notice. Speak to your doctor directly with any questions you may have regarding a medical condition. Any information contained herein does not replace any care plan as determined by a physician.
¹Birth rate percentage using aggregate data from ALL age groups on the Live Births Per Intended Egg Retrieval (ALL EMBRYO TRANSFERS) of Patient's Own Eggs chart for 2020. Reference: PFCLA SART | NATIONAL SART
© 2024 PFCLA. All Rights Reserved. Privacy Policy.